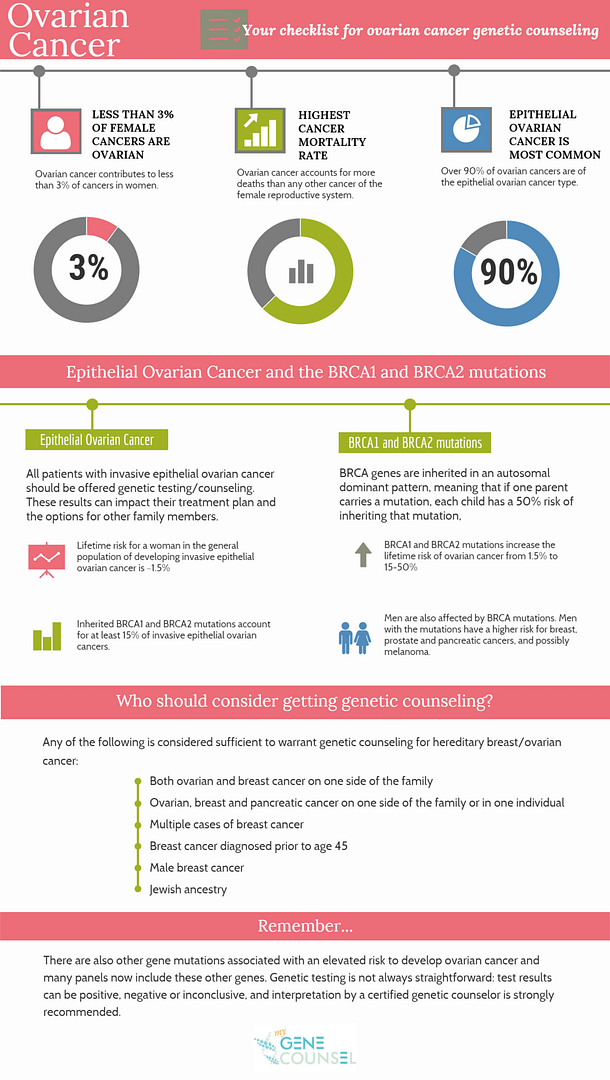
Less than 3% of cancer in women is ovarian in nature, but ovarian cancer accounts for more deaths than any other cancer of the female reproductive system. Epithelial ovarian cancer is the most common type of ovarian cancer, accounting for 85-90% of ovarian cancers.
All patients with invasive ovarian cancer (this include fallopian tube and primary peritoneal cancer) are candidates for genetic counseling and testing as the results can affect their current and future medical care, as well as their family members’ health. Germline pathogenic BRCA1 and BRCA2 variants, meaning pathogenic variants (mutations) that can be inherited, cause at least 15% of invasive ovarian carcinomas. Pathogenic BRCA1 and BRCA2 variants increase the lifetime risk of ovarian cancer to 15-50% compared to the lifetime risk for a woman in the general population of 1.5%. If a parent has a pathogenic BRCA variant, each of his/her children has a 50% risk of inheriting that variant.
Importantly, women are not the only ones affected by pathogenic BRCA variants. Men with these pathogenic variants have a higher risk for breast cancer, prostate cancer, pancreatic cancer, and possibly melanoma. Genetic testing information can help family members know more about their cancer risks, as well as their options for early detection and risk reduction for these and other cancers.
There are other genes linked with an elevated risk of developing ovarian cancer, and many multigene panels now include these other genes. Genetic testing is not always straightforward. Test results can be positive, negative, or inconclusive. Interpretation by a certified genetic counselor is strongly recommended.
Topics that should be reviewed in a genetic counseling session about ovarian cancer include:
- Personal history of cancer
- Family history of cancer
- Risks, benefits, and limitations of genetic testing
- Costs and insurance coverage for genetic testing
- BRCA1, BRCA2, and other genes linked with ovarian cancer
- The correlation between having a pathogenic variant in one of these genes and risk for ovarian and other cancers
- Whether genetic testing should be done, and if so, who the best person is to begin testing (usually the person who has ovarian cancer)
- Reviewing the possible results of genetic tests and what each result would mean
- How results could affect other family members
People who do not have ovarian cancer themselves should consider seeking genetic counseling if they have a significant family history of ovarian cancer. The following family history features may warrant genetic counseling and potentially testing for hereditary breast/ovarian cancer:
- Ovarian cancer
- Three or more cases of breast cancer
- Breast cancer diagnosed prior to age 50
- Male breast cancer
- Metastatic prostate cancer
- Pancreatic cancer
- Multiple cases of above cancers on one side of the family or in one individual
- Jewish ancestry

