Genetic Counseling Note:
People who have a mutation in one of their two CDH1 gene copies have a syndrome called Hereditary Diffuse Gastric Cancer (HDGC). This syndrome increases the risk of developing stomach cancer in men and women, lobular breast cancer in women, and may be related to other types of cancer as well. People who have a CDH1 gene mutation have options for screening and prevention. However, screening for gastric cancer is not very effective. It is hard to detect the cancer, even at a late stage, when it is not curable. Recommendations for individuals with a CDH1 mutation include considering having their stomach removed preventively in their 20-30s. Females who have a CDH1 mutation are also at increased risk to develop lobular breast cancer, and screening for breast cancer is much more effective.
November 2018 Update
Happy Stomach Cancer Awareness Month! I come into November as thankful as ever for my health and wellness. Other than a little bump in the road earlier this year, I have been feeling great. In April I was hospitalized and learned that not all food passes through when your esophagus is connected to your small intestine! After an abdominal ultrasound, CT scan, barium swallow study, and upper endoscopy, whatever was stuck there seemed to finally pass through my digestive system. Later this summer I spent a day back at Memorial Sloan Kettering Cancer Center for another endoscopy to evaluate an abnormal looking patch of cells in my upper esophagus. Thankfully, it turned out to be just normal tissue and nothing to worry about. We’re happy that’s behind us, for sure.
In January, I left my full-time job and started a new part-time position as a PA in oncology. I now care for women at risk for gynecologic cancers, with a focus on preventing ovarian and uterine cancer. I meet many women with mutations in one of the BRCA or related genes, and I love that I can understand and identify the challenges they are dealing with and can help guide them through the process of cancer surveillance and prevention.
In the fall, I was nominated by my breast oncologist to serve as the honorary walk chair for the 2019 Walk Across Southeastern Connecticut for the Terri Brodeur Breast Cancer Foundation. On October 6th, my oncologist and I walked 13.1 miles together, joined halfway through by my mom and husband. We had a great day and met some wonderful breast cancer patients, survivors, and supporters. I have been asked to join the Board of Directors for the organization, and am hoping to walk the full marathon next October!
I was also asked to participate in the next update of the International Gastric Cancer Linkage Consortium (IGCLC) Guidelines update meeting for HDGC that will be held at the University of Otago in Wanaka, New Zealand in March 2019. I will be participating in the patient, family and nutrition part of the meeting. I will have the opportunity to meet the geneticist who discovered the CDH1 gene associated with HDGC, other families affected by HDGC, and the Maori tribal families from New Zealand, where the gene mutation was first identified and will also get to visit my best CDH1 friend, Kirsty, and tour her hometown in Australia!
In reflecting on the past year, I can honestly say that despite the challenges that I have had along the way, my life has been enriched by the people I have met and the experiences I have had due to my CDH1 journey. It has been 10 years since my genetic diagnosis, and I still vividly remember the day of my genetic test results. There have been ups and downs in the process, but I know how fortunate I am to have had an early genetic diagnosis, giving me the opportunity to manage my risks of both gastric cancer and breast cancer.
Welcome Johanna, we are so glad to have you back for a third installment of your journey. In your first interview with us, you had recently learned that you have the CDH1 mutation that had been found in your father in 2007. The last time we talked (Episode 10 of Cancer Bytes Podcast), you were 26 years old, nine months out from having your stomach removed to reduce your risk of stomach cancer, and were doing very well. You are now 32 and almost 6 years out from your surgery. Fill us in – how are you now?
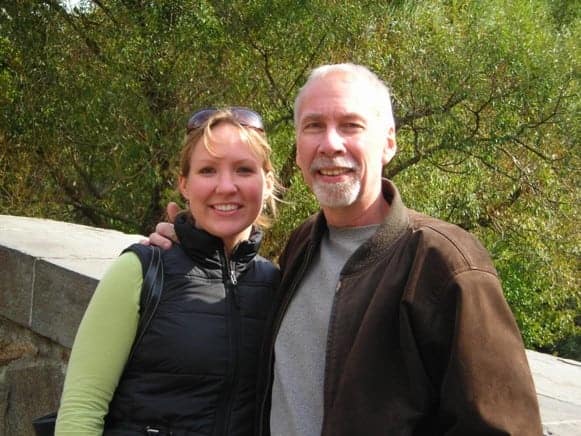
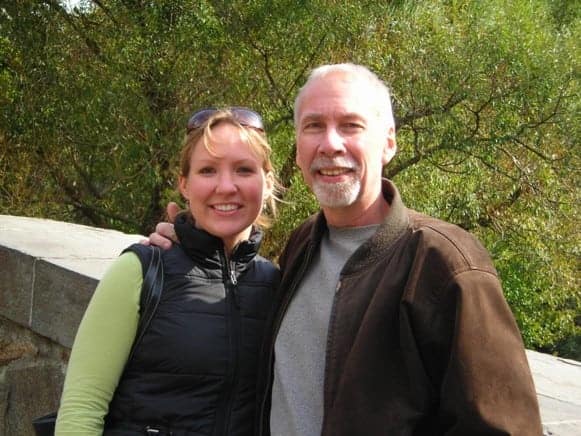
My Dad and me at one of our last visits together in NYC before he died in 2009
Things have been good. I am extremely grateful that I had a successful (prophylactic gastric) surgery with no surgical complications and a relatively quick recovery. The fact that I don’t have a stomach has become such a part of my life that it is hard for me to remember what life was like with a stomach. For example, I sometimes say I can eat whatever I want, which is really not true. There are still foods that I have trouble with, but these things have become so routine to me that it feels normal. I have a pretty healthy and active life.
When I look back at the time surrounding my gastrectomy and recovery time, it was such an intense time period. I was totally focused on the cancer risks and the steps I need to take for cancer prevention, and rightfully so – I watched what my father experienced with his diagnosis. All of my energy was directed toward getting through the surgery and recovery.
However, now almost six years out, I am managing the long-term impacts of that surgery. I am anemic (low iron levels) and have nutritional and vitamin deficiencies. I have to monitor my bone health. And I’m only 32. I don’t think about these things every day, but they do weigh on me. I will never be carefree about my health – there will always be something to worry about. It’s a bigger deal than I thought it would be.
There have been few surprises along the way, tell us about those.

A walk that Tom and I took the day I was diagnosed with Lobular Breast Cancer (Good Friday, April 3, 2015)
The first was the pathology after having my stomach removed. Many of my family members’ who had the surgery before me had pre-cancers identified in the tissue of their stomach after having ‘preventive’ surgeries. In some ways, I think I was expecting to learn the same. However, two weeks after my surgery when I got my pathology back, it revealed that I had 32 areas of pre-cancers – much more than any of us had anticipated. When I’m dealing with the side effects of this surgery, this is a helpful reminder that I made the right decision. It certainly saved my life.
The second surprise was that I was diagnosed with breast cancer at age 31, just six months after getting married. My cancer diagnosis so soon into our marriage certainly changed our relationship, and we’ve become stronger for it. But never the less, it was a challenging time and has changed us both. My original plan was to begin breast screening at age 35 because of the increased risk for breast cancer associated with a CDH1 mutation. However, after a conversation with my clinician, we decided to begin at age 30 (which has since become the recommended age to begin screening for female CDH1 carriers). If we hadn’t made that decision to start screening early, my breast cancer would have been much more advanced by the time it was detected. My breast cancer was stage 1, and I chose to have a bilateral mastectomy with reconstruction.
You’ve had two major surgeries: a gastrectomy and a bilateral mastectomy. How did they compare?

Tom and me in the hospital on the day of my mastectomy

Tom and me at his graduation from Medical School, May 2015, 2 weeks after my mastectomy
I’ve actually thought quite a lot about this, and I think the answer will surprise you. I found the bilateral mastectomy to be harder, both physically and emotionally.
When I had my gastrectomy, the hospitalization period was longer, but after about one week the pain was pretty much gone. I was able to go back to the gym and return to many of my normal physical activities within a month. The biggest challenge from that point on was learning how to eat again.
After my mastectomy, though, the physical pain lasted much longer, and I had difficulty doing daily activities independently for two to three months. Any movement that involved my upper body was difficult and painful. I had trouble turning doorknobs, brushing my own hair, driving my car, and sleeping. The emotional impact from this surgery was also greater. It has impacted my sexuality and my self-image. When I have clothes on, I think I look pretty good. But when I’m home looking at myself in the mirror, I see my body is scarred. It is a constant reminder of two very difficult times in my life.
In your first interview, you discussed your biggest concern after learning you have this mutation. It wasn’t for yourself, but what it will mean for your future children. How has that conversation evolved over the past years?

Tom and me with the PGD DNA kit from Genesis Genetics lab in Michigan
Yes, it’s tough. Really tough. I have always planned to have children. Now, family planning is much more complicated. As part of my breast cancer treatment plan, I am taking a medication, tamoxifen, for at least 5 years, and I can’t become pregnant while taking the drug due to its possible toxicity to a fetus. Pregnancy after gastrectomy can also be complicated, mostly from the nutritional point of view. It is definitely possible, just complicated. There is also a 50% chance of passing on this mutation on if my husband and I have children naturally. We’ve learned a lot about a procedure called preimplantation genetic diagnosis (PGD) that is used with in vitro fertilization to create a fertilized embryo and test it for the CDH1 mutation before it is implanted. We feel very fortunate to have this option and hope to utilize if/when we are able to have children. Although, sometimes I wonder if my body has already been through too much. Could it handle a pregnancy? Do I have the stamina? It is more than frustrating to see the idea of having children and building a family turn into a dream that may or may not happen.
What advice do you have for others?

My Mom and me doing the “HOPE” painting October 2016
When I’m faced with a challenging situation, I try to remember that it is temporary and that time will likely make it better. For example, every once in a while I will make a mistake and eat something I shouldn’t or eat too much. I’ve only “overeaten” a handful of times in the past 6 years, but I can remember each time vividly. I feel so extremely full I have to spit up or throw up, and it’s painful. I can literally feel the food in my throat. But if I give myself time, even just 20 or 30 minutes, I know it will pass. These times can be scary, too, because you’re just not sure what is going to happen and how long it will last. Over time, I’ve learned more about my new body and urge others to give themselves time to understand their new bodies as well. I like the mantra “this too shall pass” – it helps me get through the tough times.

My Dad and me at Relay for Life
I also encourage everyone with a CDH1 mutation to connect with others. Sometimes your clinician can help you do this within your own community, and there are so many ways to find others on social media. Connecting with others who understand what you are going through is extraordinary. CDH1 carriers are often faced with complex decisions at a young age. It’s a lot to handle and can feel isolating and scary. However, when you do connect with others, remember that no one person’s experience is exactly like yours. There are certainly some commonalities, but remember that your journey through decisions, surgery, and recovery will be your own and unique in many ways. In addition, you need to rely on your support system – your family, friends and medical providers. Therapy can also be very helpful to clarify your thoughts and decisions. It is a journey and no one can do it alone.
Resources:
Parts of Johanna’s decision to have a gastrectomy had been documented in the film “My Decision” available on Netflix.
Johanna’s Aunt is the founder of No Stomach For Cancer to support research and unite patients. More information about the organization a Johanna’s family’s story can be found here.