“The Forum on Healthcare Innovation: Technology and the Future of Healthcare Delivery” was hosted by Jackson Laboratories in Farmington, CT on the UCONN Health campus on October 25-26, 2017. The conference was full of healthcare innovators and professionals and covered genetic testing (including direct-to-consumer), genomics, the microbiome, patient advocacy and healthcare technology. Check out some highlight from presentations below.
Francis Collins, MD, Director of National Institute for Health, shared that the NIH also stands for hope. Reasons for hope include uncovering life’s foundations, translating discovery into health and moving forward together. Collins gave an overview of the different projects ongoing at NIH, starting with the backstory of the Human Genome Project when the human genome was first sequenced. A major aspect of the project that has impacted the future of research and healthcare was data sharing. Every 24 hours, new data collected from the day was uploaded, allowing researchers to start using the data in their own research. It would have taken years if the project researchers had waited to release data. This idea of data sharing has increased collaboration between scientists, accelerating the rate of research and development.
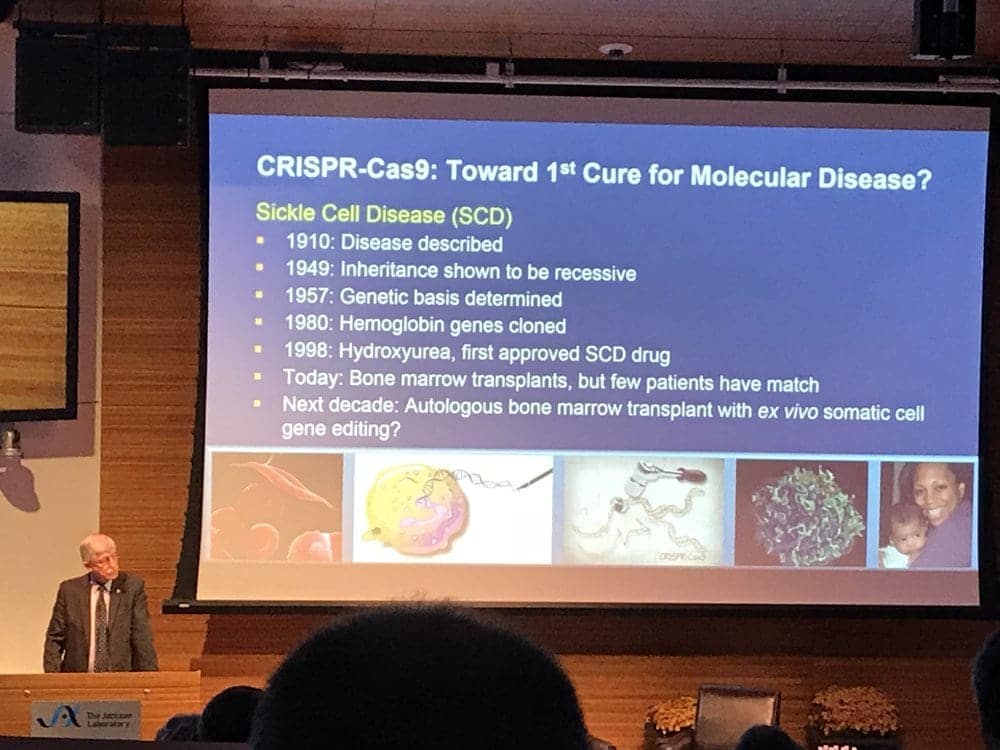
Collins also shared his excitement around CRISPR, the gene editing technology, from basic research to human trials. Basic research funds are often questioned by those not working in science. But CRISPR validates the value of investing in basic research, as an example of when a new basic research discovery completely changes healthcare. CRISPR has already achieved the status of a revolution in medicine and biotechnology. Collins predicts it will cure the first molecular disease, Sickle Cell Disease.

The current major NIH project is “All of Us” (formerly Precision Medicine Initiative). The beta stage started in May 2017 with a full launch in Spring 2018 where it will ramp up to having over 100 locations. The purpose of the project is to accelerate healthcare, specifically for individualized care by enrolling one million participants and studying their samples and big data. The term ‘participants’ is key, as opposed to ‘human subjects’, because the participants are partners in this journey. Why now? One main reason is the insane drop in the cost of sequencing: in 2004 it cost $22 million to sequence a genome. In 2017, the cost is a mere $800! “We don’t have a healthcare system, it’s a sickcare system” Collins explained. The more data we can provide showing prevention is more effective than treatment, the better we can make this transition in our health care approach.
Collins also commented on the exciting new field of microbiome research, studying the bacteria that live in and on us. Human Microbiome Project’s mission is to generate resources for comprehensive characterization of the microbiome. It started in 2008 and is now in its second phase. George Weinstock, a professor at Jackson Laboratories, stated there are 754 studies on clincialtrails.gov (as of 10/25/17) that list the microbiome. New genetic sequencing technologies (like Next Generation Sequencing) has driven this field and there are research centers focusing on the relationship between disease and the microbiome. The microbiome has additional obstacles when researching, compared to genomics, due to its enormous plasticity. Our microbiome changes with our environment, diet, etc. One interesting research study mentioned studied Olympic level athletes to find out if there is a “golden microbiome”; so far they have found a bacteria in common with many of these athletes, M. smithii. Another advancement in the field is an FDA approved product produced from microbiome research data, AEObiome’s MotherDirt. It is a body spray that is designed to be compatible with the microbiome of the skin that improves skin conditions, like acne and eczema.
James Lu, Co-Founder and Senior Vice President of Applied Genomics, Helix, discussed direct to consumer genomics and a few interesting new genetic themed apps (Neanderthal by Insitome, BABYGlimpse by HumanCode). He also talked about emerging platform for participatory research such as Precise.ly, which tracks symptoms and diseases.
Andrew Ury, Chief Executive Officer and Founder of ActX, explained how direct-to-consumer genetics can be used for potential screening for drug compatibility (pharmacogenomics). 90% of patients have potential drug genomic interactions. This is especially useful for mental health medications.

Lisa Anderson, Co-Founder and Chief Executive Officer of Genome Medical, stressed the potential genetics/genomics medicine has to improve patient outcomes and reduce costs of care, YET it’s not accessible to all patients. Genetic testing is growing 20-25% yearly; however, the workforce is only growing by 3%, resulting in a continuously growing gap. Her company aims to reduce this gap by providing real-time access to genetic counseling. Anderson also predicts within 5 years every cancer patient will have germline and somatic sequencing.

